Last updated:
‘"The smallpox on Ballarat": nineteenth-century public vaccination on the Victorian goldfields’, Provenance: The Journal of Public Record Office Victoria, issue no. 16, 2018. ISSN 1832-2522. Copyright © Nicola Cousen.
This is a peer reviewed article.
This article seeks to examine public health issues on the Victorian goldfields during the 1850s and 1860s, concentrating on the colonial experience of vaccination against smallpox on the Ballarat goldfield. It explores the history and development of vaccination, the role of the Central Board of Health, the medical profession and the public vaccinator in trying to prevent the spread of disease. Records of public vaccination, mortality and infection on the Ballarat goldfield in the initial gold rush decades, along with municipal council minutes and correspondence, are utilised to gain a clearer understanding of Victorian colonial medical practice on the goldfields.
This article examines public health issues on the Victorian goldfields during the first two decades of the gold rush through a focus on the colonial experience of vaccination against smallpox on the Ballarat goldfield. During the nineteenth century, vaccination was considered a key factor in controlling smallpox infection in the event of an outbreak in Victoria. Its implementation was successful thanks to the efforts of public vaccinators and their medical colleagues and powerful professional and local networks. The history and development of vaccination is explored, along with the roles of the central and local boards of health, the medical profession and the public vaccinator in trying to prevent the spread of disease. Victoria was a leader in the Australian colonies in public health in terms of the comprehensive manner in which vaccination policy was implemented. The public vaccinators in Ballarat serve as an example of practices that were common to all public vaccinators throughout the colony; however, they also reveal public health issues that were distinctive to the goldfields. The birthrate in this community climbed as more women arrived after the initial gold rush years, thus increasing the vulnerable immunologically naive population. Gaining a clearer understanding of colonial medical practice on the Victorian goldfields, as well as the difficulties of maintaining public health, illuminates the experience of nineteenth-century medicine throughout Australia.
Records of public vaccination, mortality and infection on the Ballarat goldfield in the initial gold rush decades, along with municipal council minutes and correspondence, and the records of the chief medical officer and the Central Board of Health (CBH) in the Chief Secretary’s Department, are utilised to gain a clearer understanding of Victorian colonial medical practice on the goldfields. Additionally, newspaper reports, medical journals, and the professional lives and practices of Ballarat doctors involved in the vaccination process from 1852 to 1869 are examined. These not only demonstrate how public vaccinators in Ballarat provided the goldfields population with a means of securing comparative immunity from smallpox, but also how vaccination policy developed. Further investigation into the records of the Chief Secretary’s Department would provide more depth to the discussion of wider vaccination issues in the early years of Victoria; however, it is beyond the scope of this article.
Public health issues on the Ballarat goldfields reflected the city’s changing population during its first two decades. In the initial gold rush years, men far outnumbered women. According to the 1854 census, there were 12,660 males living in Ballarat and 4,023 females—with females representing only 24 per cent of the population.[1] This differed from Melbourne and Geelong where females represented 44 per cent and 41 per cent of the population, respectively. The leading causes of death in Victoria at this time were zymotic diseases—that is, contagious diseases. The highest mortality rates in the colony were reported as being from dysentery and typhus (later diagnosed as typhoid or ‘colonial fever’—a diarrhoeal disease that was the scourge of the goldfields), followed by phthisis (tuberculosis) in areas outside of Melbourne.[2]
Ballarat was constituted a municipality in December 1855. When the Public Health Act 1854 was extended to encompass the district in July 1856, a Local Board of Health (LBH) was established.[3] After Ballarat East was proclaimed a municipality in May 1857, the former Ballarat municipality became known as Ballarat West. Women constituted 35 per cent of the population in Ballarat West in 1857; by 1861, the ratio was closer to equal at 44.8 per cent.[4] This was nearly double the 1854 ratio of women to men. In Ballarat East, the percentage of women was 39.8.
As more women arrived and the goldfields population became more settled, the birthrate climbed. By 1861, children under the age of 10 constituted 30 per cent of Ballarat West’s population and 27 per cent of Ballarat East’s population.[5] The leading cause of disease continued to be contagious diseases; however, the number of children’s illnesses and deaths became more prominent with these demographic changes. Childhood diseases and birth-related conditions joined gastroenteritis and diarrhoea as the leading causes of death in the district for 1863, followed by diphtheria.[6] Other large contributors to the mortality rate were marasmus (the undernourishment of children), scarlatina, premature birth, protracted birth, malformation and dentition (diarrhoea attributed to teething). Not only was there a larger infant population, but also new diseases introduced to this population could have a devastating effect, as was the case with diphtheria. As Janet McCalman and Rebecca Kippen assert, infections that survived the long voyage to Australia produced severe effects on the immunologically naive colonial-born population.[7] In the case of diphtheria, there was no vaccination in Australia until the twentieth century; however, smallpox was different.
Smallpox inoculation and vaccination
The World Health Organization has described smallpox as ‘one of the most devastating diseases known to humanity’.[8] Acutely contagious, it was transmitted by contact with infected people and, to a lesser extent, through contact with contaminated clothes and bedding. The disease entered the body through the respiratory tract and caused mouth and skin lesions. People became unwell 10–12 days after exposure to smallpox, suffering fever, headache, myalgia and vomiting. Two or three days after the fever began, a characteristic rash developed that progressed to pustules, which turned to scabs and separated after one to two weeks. Some sufferers were able to recover; however, for many, the next stage was death.
Smallpox no longer occurs naturally; it was declared globally eradicated in 1980. However, in the nineteenth century, it formed a very real threat to the wellbeing of the inhabitants of Victoria. Unvaccinated populations in which the disease had not previously existed were hit hardest. Its impact on the Aboriginal population was brutal. Richard Broome estimates that up to 60 per cent of the exposed Victorian Aboriginal population before the 1830s died from the disease.[9] Devastation from the disease was also part of the collective memory of immigrants to the colony who had experienced it in their home countries.[10] Deborah Brunton’s research shows that, during the eighteenth century, smallpox accounted for 8 per cent of deaths in Sweden, Finland and London, and 21 per cent of deaths in Dublin.[11] Further, Elizabeth Fenn contends that a smallpox outbreak in North America from 1775 to 1782 (which coincided with the American Revolution) took more lives than the war.[12]
Inoculation was introduced to England and Ireland as early as 1721 as a means of inducing immunity to smallpox. This helped to reduce the mortality rate from smallpox during the eighteenth century; however, historians are not in agreement on the extent of its effectiveness. Inoculation could be achieved by applying scabs or pus (lymph) from an individual infected with smallpox (the variola virus) to broken skin to develop a milder form of the disease and induce immunity. This was called variolation. In a modified form of inoculation, the lymph matter of humans or animals—such as calves infected with cowpox (the vaccinia virus)—was used. This was called vaccination. Variolation meant that patients had to endure a case of smallpox in an attempt to acquire immunity. By contrast, through vaccination, immunity might be acquired without suffering a case of the disease.
Vaccination was generally introduced to the skin by piercing through a drop of vaccine, rubbing vaccine into an incision or using a vaccine-charged instrument in one or multiple sites. The effectiveness of the vaccine depended on the potency, the virus strain, its preparation and storage conditions, and the extent of bacterial fungal and viral contamination from lymph harvested from live animals.
Nineteenth-century Ireland provides an example of the success of vaccination in a country where smallpox was endemic. Legislation was introduced to make vaccination free in 1851 and compulsory in 1863. The mortality rate from the disease dropped from 854 in 1864 to just 20 in 1869. Despite virtually identical legislation in Ireland and England, the compulsion to vaccinate was more successful in Ireland. Deborah Brunton attributes this to the work of medical practitioners.[13] Medical practitioners were to play an important role in the success of vaccination in Victoria too.
Vaccine lymph was distributed to the colonies through the avenues of empire. It was transported to Australia on board ships through arm-to-arm transmission using human lymph. Human lymph was mostly used in Victoria before 1880, after which the usage of calf lymph became more common. This was largely due to concerns about transmission of childhood diseases and syphilis during the operation, as Alison Bashford suggests.[14] Lymph was distributed to Victorian country areas on glass wrapped in moist paper and oiled silk by the registrar-general and, later, by the chief medical officer.[15] Over 300 charges of vaccine lymph were distributed throughout the colony in this manner in the second half of 1858. Vaccinators helped to determine how long the lymph remained effective through this distribution method as the practice developed in Victoria and distribution methods improved.
Vaccinators in Ballarat received their vaccine supplies from three sources: government medical officials, other doctors and lymph taken from children they had vaccinated. Children were required to return to the vaccinator eight days after the operation to check whether the vaccine had taken. During these visits, vaccinators issued vaccination certificates and took lymph for use in future vaccinations, thus maintaining their vaccine matter supplies (see Figure 1). Sometimes, multiple attempts were required for a vaccination to take, with some in Ballarat not working after seven attempts.
Figure 1: Certificate of successful vaccination 1858 signed by Dr James Stewart, the public vaccinator for Ballarat, 79.0695: Vaccination Certificate, Gold Museum (The Sovereign Hill Museums Association), Ballarat.
The Victorian Compulsory Vaccination Act 1854 and the public vaccinators
The influx of highly educated middle-class immigrants during the gold rush, many of whom expeditiously established institutions, meant that Victoria developed differently to other Australian colonies. The relative modernity of Victorian public health is reflected in the speed at which the colony adopted medical advances and legislation following changes in the United Kingdom. Victoria’s CBH was established soon after its counterpart in England and Wales. This differs greatly from public health in New South Wales where the first Board of Health was not established until 1881 when public and political demand was spurred by a smallpox epidemic.[16] Victoria established high quality vital registration, some quite modern hospitals and a medical society and journal by the 1860s. In contrast, New South Wales had no permanent professional medical association or journal until the 1880s.[17] Ballarat followed the broad pattern of Victorian public health, but was also addressing the distinctive health needs of the goldfields community. By 1860, Ballarat’s visionary pioneers had established a public hospital for miners, an LBH (after the establishment of Ballarat’s first municipal council) and a benevolent asylum.
Australian colonies followed different courses with their vaccination enforcement. As Rebecca McWhirter asserts, ‘Victoria both enacted and enforced compulsory vaccination; Tasmania passed, but failed to consistently enforce, similar legislation; and New South Wales never imposed compulsory vaccination’.[18] Victoria’s Compulsory Vaccination Act 1854 made vaccination compulsory in the colony. It followed the United Kingdom Vaccination Act 1853, which mandated the vaccination of infants born in England or Wales. Examination of correspondence between Dr William McCrea, who was both chief medical officer of Victoria and president of the CBH, and the Chief Secretary’s Department, provides insight into many facets of the decision-making process involved in vaccination policy. Elements of these records are echoed in contemporary newspaper reports; however, the records provide greater context and extra detail of the human agency involved in the process. They highlight the efforts of some doctors in their fight to protect the Victorian population from potential smallpox outbreaks, as well as opposition to those measures. For example, prompted by the prevalence of the disease in Mauritius, McCrea sought to organise a vaccine facility in Melbourne as part of the Act.[19]
Under the 1854 Act, the colony was divided into 28 vaccination districts and 28 public vaccinators were appointed.[20] By 1862, the number of public vaccinators had climbed to 144, reflecting the needs for disease control in the burgeoning population.[21] As in Ireland, England and Wales, it became illegal to perform inoculations in Victoria, as this kept the smallpox disease in circulation. Bashford contends that ‘replacing inoculation with vaccination was part of the mission of imperial medicine’[22]—a mission that was enlarged through the spread of smallpox to isolated communities as part of imperial expansion in the first place.
Any medical practitioner legally qualified in the colony under the Medical Practitioners Act 1854 could perform vaccinations and this continued to be the case after public vaccinators were introduced. Philippa Martyr suggests that public vaccinators appointed ‘in outlying districts were generally lay people, as they were more likely to abide by the letter of the law’.[23] However, this does not adequately reflect the experience in Victoria. There were a few cases where laypeople were made vaccinators for districts where no registered practitioner was available, but this was problematic, brief and not the practice in the majority of cases. For example, laypeople were appointed vaccinators in 25 districts in 1865 and the vaccinator for two of these places had already been struck off for non-compliance with the Act.[24] Some doctors were concerned that ‘unqualified medical men’ holding the government appointment of vaccinator were ‘falsely assuming the title of “Doctor”’ and misleading the public ‘who believed they must be “bona fide Doctors”’.[25] As David Evans suggests, the practice attracted ‘fierce opposition from the medical profession’.[26] Doctors had to fight hard to protect their professional status and incomes in the years prior to medicine’s professionalisation in Victoria.
The public vaccinators of Ballarat
Appointed in December 1854, Ballarat district’s first public vaccinators were Dr James Williams (at Ballarat) and Dr James Graham (at Buninyong).[27] Williams was soon replaced by Dr James Stewart who remained the public vaccinator for Ballarat until he left the colony in 1869. Public vaccinators were appointed in other parts of the district as the population grew (see Table 1). These included Dr Henry Leman (at Ballarat East), Dr Louis Saenger (at Smythesdale), Dr William Bailey Rankin (at Buninyong), Dr John Aucterlonie Creelman (at Learmonth) and Dr Henry Crossen (at Carngham). Reflecting Ballarat’s melting pot of nationalities, they came from a range of countries—including Ireland, England, Scotland and Saxe-Weimar—and brought with them different levels of medical education, understanding and experience.
|
Ballarat: Buninyong: Smythesdale: Ballarat East: Gordon’s and Mount Egerton: |
Learmonth (and, later, Burrumbeet and The Springs): Carngham: Durham Lead: Sebastopol: Warrenheip: |
Table 1: Public vaccinators for Ballarat and district during the 1850s and 1860s
During the 1850s and 1860s, Ballarat’s public vaccinators were some of the leading doctors of the area. Men of influence in their community, many were popularly elected to honorary hospital and public positions. Most had travelled to Victoria as ship’s surgeons and this formative experience influenced the goldfields medicine of Ballarat as well as its civic development. This was because ship’s surgeons had many duties in addition to medical care. To maintain the health and wellbeing of passengers on their voyage to Australia, ship’s surgeons were responsible for controlling discipline, sanitation and spaces on board the ship. Some Ballarat doctors, such as Stewart and Clendinning, were also municipal councillors and, thus, were members of the local boards of health. Council minutes, central and local boards of health correspondence, and health reports, are integral to understanding the ways in which communication between government bodies at colonial and local levels and doctors served to influence disease control measures. Councillors sat as the LBH at the end of council meetings, but health issues and correspondence from the central and local boards of health were also addressed during council meetings.[28] It was through these local boards that the CBH effected its measures. There were just five local boards when sanitary administration began in Victoria in the 1850s; however, by 1871, there were 166 local boards of health.[29]
The reach of public vaccinators extended well beyond their official role into a wide range of medical positions in the community. For example, the introduction of public vaccinators in Victoria coincided with measures of the newly formed Ballarat Medico-Chirurgical Society to protect the goldfields population from ‘quacks’. The first list of qualified practitioners was published in the Ballarat Star on 1 January 1855, the day the Compulsory Vaccination Act took effect. This also served to direct business to the listed doctors. Through forming professional groups, medical practitioners increased their power and status in the district, and strengthened their networks, which enabled them to take on other public positions.
Vaccination was embraced by many people in the Ballarat district. From the commencement of the Compulsory Vaccination Act in January 1855 to March 1861, 7,738 children were vaccinated in the district; another 2,914 were vaccinated in Ballarat over the following two years.[30] Yet, vaccination rates were never close to universal for Ballarat or for the entire colony and not everybody conformed to vaccination laws. The public vaccinators could employ a variety of means to encourage people to vaccinate their children. If they failed to do so, or did not return after eight days to check if the operation was successful, parents or guardians could be fined up to 40 shillings for the first offence and up to £5 for further offences.[31] In March 1861, Dr Stewart took John Graber to court for not bringing his child back to check whether the vaccination had taken effect.[32] Stewart did not wish to press charges; instead, he used the occasion to alert the public that they had to comply with the Compulsory Vaccination Act.
The strong networks and connections of the Ballarat doctors helped the vaccinators to influence public health. Many public vaccinators in Ballarat were also accoucheurs—doctors trained in midwifery—and, as such, could influence the vaccination of infants for whom they had been the birth doctors. They worked closely with the deputy registrar for Ballarat, William Pooley. Pooley regularly placed warnings in the Ballarat newspapers that parents and guardians who neglected registration and vaccination risked fines or imprisonment. He also took people to court for not vaccinating their children within the time prescribed by law.
Children were supposed to be vaccinated by six months of age, although Ballarat doctors also vaccinated children who were much older. Sometimes, older children were vaccinated for the first time with their younger siblings; consequently, in the event of an outbreak, there were children of varying ages who were susceptible. The CBH recommended that adults who had not been vaccinated for over 10 years get revaccinated, particularly during times of suspected outbreaks.[33] Vaccination registers provide important insight into how closely the vaccinators followed vaccination policy. Ages of vaccinated people listed in the extant vaccination registers for the Ballarat district during the 1860s range from five weeks to 19 years.[34] This indicates that most, if not all, of these vaccinations were first time vaccinations and not the revaccinations of adults. However, this is only an indication of vaccination practices, as the registers held by the Public Record Office Victoria are not complete for the district or for all years. For example, the important 1850s registers are missing and there are no registers for Dr Stewart’s vaccination office or the Ballarat East vaccination office. This is a large gap in the data, as Stewart was the longest standing public vaccinator for the district during this period and his clinic remained the most popular, even after other newer clinics were more readily accessible to patients. For example, Dr Leman claimed that few children visited his vaccination office in 1858 because most attended Dr Stewart’s office for vaccination.[35]
Figure 2: Register of certified cases of successful vaccination in the district of Bungaree, 1868, PROV, VPRS 3654/P1, Unit 1, Registers of Vaccination.
The registers provide details of the child’s name, age, father’s name, address (town/district) and the name of the vaccinator, occasionally with some remarks. Unfortunately, they do not list how many attempts were required for each child’s vaccination to work. Although public vaccinators would be the vaccinator for the majority of children in their district, the registers confirm that a number of other vaccinators were vaccinating children within the same district. Most of the extra vaccinators were from nearby areas, but some came from further afield. For example, Dr JTB Laurie was the public vaccinator for Learmonth in 1869 and, along with local doctors JA Creelman and John Fishbourne, he vaccinated the majority of children in the register. In the same register, there were also vaccinations performed by Dr Steel at Creswick, Dr Robinson at Clunes, D Fowling at Talbot, WH Hinchcliff at Mortlake and George Crowlands at Inglewood.
Central Board of Health measures against the spread of smallpox
Smallpox came to Victoria during the 1850s aboard immigrant ships. Thereafter, the risk from infectious diseases was redefined by the technological transformation of the seaways, as Peter Hobbins argues.[36] The chief medical officer’s correspondence provides useful insights into the experiences of health and quarantine measures involved in attempts to keep Victoria free of smallpox. The Ocean Chief had 14 cases of smallpox during its voyage to Victoria in 1857 and was held in quarantine off Point Nepean after its arrival in Port Phillip on 26 June.[37] About 340 passengers (excluding saloon passengers) were removed to the sanitary station under the control of the chief medical officer. By waiting for no more infections to occur, the disease was prevented from entering the colony, despite the failed attempt of saloon passengers to be excused from such quarantine measures.[38] However, the disease circumvented quarantine measures three months later, resulting in three deaths. The infection was spread by three passengers from the Commodore Perry, which arrived at Port Phillip Heads on 12 September 1857 from Liverpool. According to the CBH, it was through ‘the wilful concealment of the presence of the disease’ and an ‘attempt to evade quarantine laws’[39] that infected passengers were allowed off the ship. It took 18 days for new suspected cases to appear in the Melbourne and Gisborne areas. The disease could spread in the colony away from the original outbreak site, as carriers may not have known they had the disease due to its asymptomatic incubation period.
When suspected cases appeared in the neighbourhood of Lonsdale and Spencer streets in Melbourne a few weeks after the ship’s arrival, the CBH considered that ‘the vaccination of all individuals (both children and adults) upon whom that operation has not been performed, a sufficient precaution against the spread of the disease’.[40] The CBH chose not to invoke the 23rd section of the Public Health Act at this time. This would have allowed them to order the cleansing, purifying, ventilating and disinfecting of houses, buildings, churches and places of assembly.[41]
Dr McCrea experienced resistance and opposition when trying to implement the CBH’s sanitary measures during the suspected outbreak. He ordered a young member of the Kirk family who was suspected of suffering from the disease to be removed from Jeffcott Street to Royal Park in October 1857. McCrea asked his companion, Dr Knaggs, to immediately vaccinate an unvaccinated child in the house ‘to prevent the disease spreading to the neighbourhood, and to prevent if possible [the] other child from being attacked’.[42] A former naval surgeon, McCrea was a strong advocate for vaccination. As Hobbins contends, British naval surgeons were both powerful advocates and instruments for vaccinating those travelling to and living in the colonies.[43]
Knaggs did not return with vaccination lymph; instead, he informed the child’s father that removal was optional.[44] Adding to public fear and misunderstandings of procedures, Knaggs wrote to the newspapers, spreading what McCrea referred to as ‘generally malignant falsehoods’ and deliberately doing ‘every thing in his power to thwart the sanitary precautions of the Central Board of Health’.[45] The parents eventually agreed to having their child removed; however, the child died within few hours of reaching Royal Park. Immediately after the child’s removal, McCrea ordered that the Kirk family’s clothes and bedding be put through boiling water and that their home be cleansed with boiling water, the walls and floors washed with diluted chloride of zinc solution. McCrea’s attempt to vaccinate the second child failed and it too succumbed to the disease.
The Medical Society of Victoria also resisted the CBH’s sanitary measures. In protest against the final enactment of the Bill for the Suppression of Small Pox in 1857, it claimed that the Bill could not ‘fail to lower the character and prestige of the Medical Profession of Victoria in the eyes of their medical brethren in the neighboring colonies and also at home’.[46] The society was concerned that medical men should not be penalised for not doing their job, that the Bill allowed unqualified men to perform vaccinations and that transmitting vaccination certificates to the registrar-general added to the medical men’s workloads (without adding to their purses).[47] However, its members supported the preventatives of general vaccination and sanitary measures, conceding that ‘small-pox cannot now be excluded from the colony by any oppressive quarantine regulation’.[48] As events played out in the newspapers, the potential for the reading public to lose faith in the CBH, thereby reducing its impact and impeding the effectiveness of its measures, was noted. Out of concern that the public might view its future work with ‘mistrust’,[49] the CBH called for an enquiry into the matter. Highlighting the important role medical men played in shaping policy—and in what probably amounted to a policy of appeasement—the CBH announced that ‘the moral influence possessed by them [the CBH], in connection with the Medical men of the city, will be sufficient to induce persons afflicted to remove to the Royal Park’;[50] no further legislation for compulsory measures was required.
The CBH’s records also reveal the extent to which financial concerns affected the effective implementation of sanitary measures to avoid the spread of smallpox in the colony. The board had a budget of £250 in 1857 (supplemented with £550) and £150 in 1858. In early 1858, it requested more money to cover expenses involved in the ‘considerable and unforeseen expenditure’ accompanying smallpox outbreaks. McCrea indicated that, unless additional money was made available, ‘the Board will not feel themselves justified in incurring any further expense which some unforseen [sic] emergency may possibly render necessary’.[51] Further, he claimed that any contrary decision would ‘so fetter its [the CBH’s] operations and cripple its usefulness by preventing that energetic action so necessary in enforcing its regulations, that the object for which the Board has been constituted will be very much, if not wholly, set aside’.[52] McCrea and other board members had contributed some of their own private money to prevent such a crippling of the board’s efficiency and operations.[53] The chief secretary promptly advocated for the CBH to receive an extra £500 for 1858.[54]
Outbreak fears in Ballarat
After the 1857 outbreak in Melbourne, local boards of health were reminded of the necessity for general vaccination as a precaution against the outbreak of the disease and of measures to be taken to suppress the disease in the event of its introduction. The CBH wrote to the Ballarat LBH with guidelines ‘for the prevention as far as possible and mitigation of epidemic or contagious disease’.[55] The municipal and Chief Secretary’s Department correspondence reveals the extent to which board communication facilitated the implementation of these measures. The public vaccinator had to be notified of all cases of smallpox and had to vaccinate all children in the neighbourhood of the cases who had not already had the operation. The infected person had to be isolated and could only be visited by medical attendants. Another person had to be found to take care of them if no relative or friend was willing to attend them, preferably someone who had already had the disease and possible immunity to it.
Conditions particular to the goldfields caused additional complications. In 1858, drainage issues in Ballarat concerned the local and central boards of health. Debris from puddling and sluicing operations (sludge) filled the beds of water courses, encroached on the roads, damaged property and interfered with drainage. In the event of a smallpox outbreak, the cleansing and disinfecting of a house or tent of an infected person would be impaired by lack of drainage and by the contaminated liquids waiting to evaporate. Ground pollution from privy cesspits could also spread disease; however, it was not until 1872 that the city’s LBH began a zealous campaign to convert over 4,000 privies to the earth closet system.[56] During the 1850s and 1860s, privies at the Ballarat Railway Station were still being flushed into the Yarrowee Creek, and there was a special channel for the flushing of the city’s hospital, bank and hotel closet cesspools.
In the wake of the smallpox outbreak in Melbourne, a suspected outbreak occurred in Ballarat that exemplifies the fear and confusion about smallpox in Australia and the varied opinions of doctors. In April 1858, an eight-year-old girl, Miss Lecki, was suspected to have contracted the disease.[57] Dr Edward Duffin Allison had been attending her and considered her conical-shaped pustules to be an aggravated case of chickenpox. Dr Walter Lindesay Richardson, who had vaccinated Lecki a year earlier, believed that she was suffering from malignant smallpox, as she was covered in pustules of various stages. In the belief that smallpox was a consequence of ‘ignorance and filth’, and despite vaccinating some of his patients, Richardson was in favour of sanitary measures over vaccination.[58] Not everyone shared his beliefs. On being notified of the case, CBH President Dr McCrea requested authority to extend the Public Health Act to encompass Ballarat East and for the Chief Secretary’s Department to incur whatever expense was required to prevent the spread of the disease.[59] McCrea also called for an investigation by the public vaccinator, Dr Stewart, and the honorary medical officers of the Ballarat Hospital, Charles Kenworthy, George Nicholson and Henry Mount. The doctors concluded that the girl had the less dangerous cowpox and not smallpox.
The Star newspaper, which misreported the case in an alarmist manner, suggested that Dr Allison was disgracefully derelict in his duty, and that he had placed the community at risk of the virulently infectious disease. A pitiable apology was given the following day; the newspaper expressed regret for having caused unnecessary alarm—if they had made a mistake, which they were not convinced they had, they were in the company of medical professionals who could not agree. The Star was entirely unhelpful; it continued to undermine Stewart and the other doctors and recommended that the 60 or 70 children who attended Miss Lecki’s school should stay at home. As public vaccinator, Stewart condemned the spread of false reports; he explained that, had he and his colleagues not investigated the case, the Lecki family’s tent and bedding would have been needlessly destroyed. If the doctors, particularly the public vaccinator, had not been so well trusted by the public, the Star could have stirred up vigilantes to burn the family’s tent and belongings, placing the sick child at risk. During the 1857 Melbourne outbreak, lodgers who shared a house with a patient suspected of having smallpox were ‘inclined to remove him by any means’.[60] The man had been refused admission to the Melbourne Hospital. McCrea had to intervene, placing the sick man in an isolated area of the Immigration Depot overnight while he made arrangements for his care and isolation from the rest of the community.[61] In actions reflecting those of the Ballarat district public vaccinators, McCrea felt that he ‘was bound by common humanity to provide for [the patient] in some way and the only means at my disposal were those I adopted’.[62]
Attempts to obtain a vaccination office for Ballarat East before the suspected outbreak in 1857 had failed, despite Dr George Clendinning’s concern that it ‘was really too much, for delicate females to undergo, the long journey through the mud of the Main-road up to the Western Township’,[63] which is where Dr Stewart’s vaccination office was situated. However, rather than out of concern for poor ‘delicate’ females, Clendinning’s motives were business-oriented. With the population and birthrate increasing, female and child patients were important contributors to a doctor’s livelihood and much business was being directed towards the doctors of Ballarat West. Dr Leman was appointed the first public vaccinator for Ballarat East following this smallpox scare.
Public vaccinators continued to play an important part in the prevention of smallpox through vaccination and in calming public fears during the 1860s. Doctors Stewart, Nicholson and Thomas Le Gay Holthouse were called to consult on a suspected smallpox case at the Ballarat Benevolent Asylum in November 1862.[64] The female patient had thick papular eruptions on her face, arms and body, which became pustular. However, the doctors all agreed that it was not smallpox. Other suspected outbreaks in the colony continued to heighten fear of the disease.
A second smallpox outbreak began in Melbourne in 1868. The disease had again breached quarantine measures, as its source was ship passengers. This outbreak lasted six months and involved 43 verified cases.[65] The chief mate of the infected ship, the Avon Vale, died from smallpox in the Immigration Hospital, as did a patient in his hospital ward. Several suspected cases were reported in the hospital neighbourhood but were determined to be chickenpox. An article in the Australian Medical Journal suggested that some cases were incorrectly diagnosed as smallpox because the people involved had ‘an inordinate craving after notoriety’.[66] A commission was appointed to investigate and its nine medical practitioners were divided in opinion: two thought the cases were true smallpox, three thought they were smallpox modified by vaccination but capable of producing true smallpox in the unvaccinated and four thought it was not smallpox at all. The lack of consensus raised questions about correct diagnoses, adding to the public’s confusion and fear.
The press and public health awareness
Victorians were kept aware of the harsh reality of smallpox through newspaper reports of mortality rates and endemic and intermittent states in their home countries and other overseas countries, as well as reports of suspected outbreaks in Victoria. There was also a good deal of scaremongering. This could be both beneficial and detrimental. Suspected outbreaks were so significant that, according to McWhirter, they ‘provided the stimulus necessary for great leaps forward in the development of public health’.[67] However, scaremongering could also be dangerous and encourage mob mentality. For example, as already noted, had the Ballarat public vaccinator’s opinion and advice not been trusted, the outcome in the 1858 Lecki case could have been dire.
Public vaccinators, registrars, the chief medical officer and the CBH also used newspapers and journals to administer the Compulsory Vaccination Act and implement precautionary public health messages and measures. Reports on court cases provided fear of punishment for not vaccinating, important news on possible outbreaks kept the public informed and medical authorities published information in attempts to dispel harmful myths and misinformation. Heightened fear from news of suspected outbreaks served to increase vaccination rates, especially when people had been lax, as had been the experience in Melbourne.
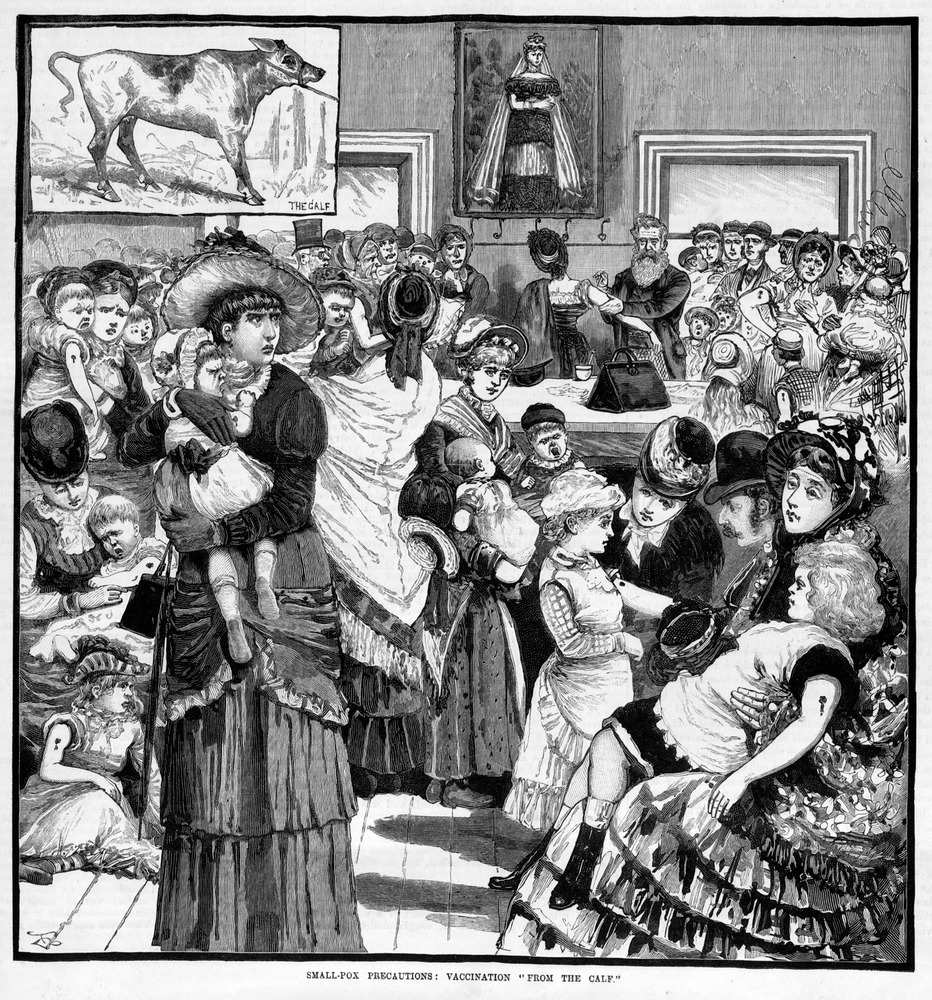
The CBH used the prevalence of smallpox in London in July 1863 to encourage parents to vaccinate their children. According to the Star, the response in Ballarat was so great that the footpath outside the public vaccinator’s office in Armstrong Street was ‘rendered almost impassable with women and children’,[68] and the vaccinator’s supply of lymph was exhausted (for example, see Figure 3). The newspaper also reported that the deputy registrar was taking out summonses against those who neglected to vaccinate their children, thus combining the fear of disease with the fear of financial loss to achieve the desired effect. The CBH began to admit reporters to their meetings in early 1869. Public health in Ballarat was more transparent and accessible to the public, as LBH meetings were always reported in the Star as part of municipal council proceedings.
Figure 3: A vaccination office crowded with women and children. ‘Small-pox precautions: vaccination “from the calf”’, Australian Sketcher, 6 May 1882.
Victoria’s two greatest protections from outbreaks of smallpox were its isolation from countries where smallpox existed and vaccination. As the 1857 and 1868 experiences reveal, immigration medical checks and quarantine measures were not a perfect barrier to the disease. The CBH considered extensive vaccination to be ‘the only means of rendering such a visitation as harmless as possible’,[69] as it secured comparative immunity from the disease.
The Ballarat public vaccinators provided their goldfields population with a means of securing comparative immunity from smallpox. They provided the knowledge and advice to allay fears, diagnosis of suspected cases (despite divided medical opinions) and the care of the community through their medical and civic roles. By such means, they earned the trust of their community, which, in turn, prevented fear from turning into panic and vigilantism. These doctors had high status in their community and the role of public vaccinator added to this status. Public health in Ballarat reflects the larger pattern of Victorian public health, which differed from other Australian colonies. However, it also diverged from this pattern, as its doctors adapted to the distinctive goldfields conditions, networks and demography. Vaccination was a key factor for controlling smallpox infection in the event of an outbreak in Victoria during the nineteenth century and its implementation was successful thanks to the efforts of the public vaccinators, the central and local boards of health, their medical colleagues and their powerful professional and local networks.
Acknowledgments
I wish to acknowledge and thank Sebastian Gurciullo and Abigail Belfrage for their generous assistance with accessing some of the Public Record Office Victoria records.
Endnotes
[1] Victoria, Census of Victoria, 1854, Government Printer, Melbourne, [1855].
[2] Victoria, Births, deaths, and marriages in the Colony of Victoria: annual report of the registrar general, Government Printer, Melbourne, [1855–1856], pp. 37, 45, 47; Janet McCalman, ‘Diseases and epidemics’, available at <http://www.emelbourne.net.au/biogs/EM00473b.htm>, accessed 13 March 2018.
[3] PROV, VA 478 Ballaarat (Municipal District 1855–1863; Borough 1863–1870; City 1870–1994), VPRS 2500/P0 General Correspondence Files, Unit 1, Health Reports 1856–1867, Public Health Act Extended to Ballaarat, proclamation.
[4] Victoria, Census of Victoria, 1861, Government Printer, Melbourne, [1862], p. 13; Weston Bate, Lucky city: the first generation at Ballarat, 1851-1901. Melbourne University Press, Carlton South, 1978, p. 106.
[5] Victoria, Census of Victoria, 1861, p. 24.
[6] ‘Vital statistics of Ballarat’, Star, 27 February 1864, p. 1S.
[7] Janet McCalman & Rebecca Kippen, ‘Population and health’, in Alison Bashford & Stuart Macintyre (eds), The Cambridge history of Australia: Indigenous and colonial Australia, vol. 1, Cambridge University Press, Port Melbourne, 2013, p. 309.
[8] WHO, ‘Smallpox’, available at <http://www.who.int/biologicals/vaccines/smallpox>, accessed 17 May 2016.
[9] Richard Broome, The Victorians: arriving, Fairfax, Syme & Weldon, McMahons Point, 1984, p. 28.
[10] Anne Hardy, ‘The medical response to epidemic disease during the long eighteenth century’, in JAI Champion (ed.), Epidemic disease in London, Centre for Metropolitan History, Institute of Historical Research, University of London, 1993, p. 65.
[11] Deborah Brunton, The politics of vaccination: practice and policy in England, Wales, Ireland, and Scotland, 1800–1874, University of Rochester Press, Rochester, 2008, p. 12.
[12] Elizabeth A Fenn, Pox Americana: the great smallpox epidemic of 1775–1782, Hill and Wang, New York, 2001, pp. 6, 266.
[13] Deborah Brunton, ‘The problems of implementation: the failure and success of public vaccination against smallpox in Ireland, 1840–1873’, in Greta Jones & Elizabeth Malcolm (eds), Medicine, disease and the state in Ireland, 1650–1940, Cork University Press, Cork, 1999, p. 151.
[14] Alison Bashford, Imperial hygiene: a critical history of colonialism, nationalism and public health, Palgrave Macmillan, Basingstoke, 2004, p. 20.
[15] Victoria, Central Board of Health, Fifth annual report under the Act 18 Victoria, No. 13, Government Printer, Melbourne, 1859–1860, p. 3.
[16] CJ Cummins, A history of medical administration in NSW 1788–1973, NSW Department of Health, North Sydney, 1979, pp. 63, 65.
[17] Milton Lewis & Roy MacLeod, ‘Medical politics and the professionalisation of medicine in New South Wales, 1850-1901’, Journal of Australian Studies, no. 22, 1988, p. 81.
[18] Rebecca McWhirter, ‘Lymph or liberty’: responses to smallpox vaccination in the eastern Australian colonies, PhD thesis, University of Tasmania, 2008, p. iv.
[19] PROV, VPRS 1189/P0 Chief Secretary’s Department, Inward Correspondence 1, Unit 133, Medical: Chief Medical Officer (Colonial Surgeon until June 1854), Coroner, 1854–, letter from William McCrea, chief medical officer, to colonial secretary, 17 August 1854.
[20] Victoria, Compulsory Vaccination Act 1854, Government Printer, [Melbourne], 1854, p. 9; Victoria Government Gazette, 26 December 1854, p. 3056.
[21] Victoria, Statistics of the Colony of Victoria for the year 1862, Government Printer, Melbourne, 1862, pp. 343–345.
[22] Alison Bashford, ‘Medicine, gender, and empire’, in Phillipa Levine (ed.), Gender and empire, Oxford University Press, New York, 2004, p. 116.
[23] Philippa Martyr, Paradise of quacks: an alternative history of medicine in Australia, Macleay Press, Paddington, 2002, p. 67.
[24] ‘Local news’, Australian Medical Journal, April 1865, p. 143.
[25] ‘Medical news’, Australian Medical Journal, July 1858, p. 240.
[26] David Evans, ‘Vaccine lymph: some difficulties with logistics in colonial Victoria, 1854–1874’, in John Pearn & Catherine O’Carrigan (eds), Australia‘s quest for colonial health: some influences on early health and medicine in Australia, Department of Child Health, Royal Children’s Hospital, Brisbane, 1983, p. 161.
[27] Victoria Government Gazette, 26 December 1854, p. 3056.
[28] PROV, VPRS 13007 Council Minutes; PROV, VPRS 2500/P0 General Correspondence Files, Unit 1, Health Reports 1856–1867, letter from Fred Thomas, secretary CBH, 5 October 1857.
[29] Victoria, Central Board of Health, Twelfth report with appendices, Government Printer, Melbourne, 1871, p. 3.
[30] ‘News and notes’, Star, 23 April 1861, p. 2; ‘Social’, Star, 23 July 1863, p. 1S.
[31] Victoria, Compulsory Vaccination Act 1854, p. 12.
[32] ‘District police court’, Star, 27 March 1861, p. 4.
[33] Victoria, Central Board of Health third annual report, Government Printer, Melbourne, 1858, p. 3.
[34] PROV, VA 2889 Registrar-General’s Department, VPRS 3654/P0 Registers of Vaccinations. Bungaree 1868, 1869; Buninyong 1864, 1865, 1866, 1867, 1868, 1869; Burrumbeet 1863, 1864, 1865, 1868; Durham Lead 1865, 1866, 1868, 1869; Learmonth 1863, 1864, 1866, 1867, 1869.
[35] ‘Eastern Municipal Council’, Star, 8 June 1859, p. 3.
[36] Peter Hobbins, ‘Union Jack or Yellow Jack? Smallpox, sailors, settlers and sovereignty’, Journal of Imperial and Commonwealth History, vol. 45, no. 3, 2017, p. 391.
[37] PROV, VPRS 1189/P0 Chief Secretary’s Department, Inward Correspondence 1, Unit 553, Medical, 1857–, letter from William McCrea, chief medical officer, to chief secretary, 17 July 1857.
[38] PROV, VPRS 1189/P0 Chief Secretary’s Department, Inward Correspondence 1, Unit 553, Medical, 1857–, letter from McKay, Baines & Co to His Excellency Sir Henry Barkly, 15 July 1857.
[39] Victoria, Central Board of Health third annual report, p. 8.
[40] PROV, VPRS 1189/P0 Chief Secretary’s Department, Inward Correspondence 1, Unit 553, Medical, 1857–, letter from William McCrea, president CBH, to Chief Secretary, 29 September 1857.
[41] Victoria, Public Health Act 1854, Government Printer, Melbourne, 1854, Section XXIII.
[42] PROV, VPRS 1189/P0 Chief Secretary’s Department, Inward Correspondence 1, Unit 553, Medical, 1857–, letter from William McCrea, president CBH, to chief secretary, 6 November 1857.
[43] Hobbins, ‘Union Jack or Yellow Jack?’, p. 399.
[44] PROV, VPRS 1189/P0 Chief Secretary’s Department, Inward Correspondence 1, Unit 553, Medical, 1857–, letter from JN Hassall, superintending inspector, to secretary CBH, 22 October 1857.
[45] McCrea to chief secretary, 6 November 1857.
[46] PROV, VPRS 1189/P0 Chief Secretary’s Department, Inward Correspondence 1, Unit 553, Medical, 1857–, paper presented by deputation from the Medical Society to His Excellency, 23 November 1857.
[47] PROV, VPRS 1189/P0 Chief Secretary’s Department, Inward Correspondence 1, Unit 553, Medical, 1857–, copy of resolution passed by the Medical Society in reference to Kirk’s child and legislation, 25 November 1857.
[48] PROV, VPRS 1189/P0 Chief Secretary’s Department, Inward Correspondence 1, Unit 553, Medical, 1857–, resolution adopted at a meeting of the Medical Society of Victoria held on 4 November 1857.
[49] PROV, VPRS 1189/P0 Chief Secretary’s Department, Inward Correspondence 1, Unit 553, Medical, 1857–, letter from William McCrea, president CBH, to chief secretary, 25 November 1857.
[50] PROV, VPRS 1189/P0 Chief Secretary’s Department, Inward Correspondence 1, Unit 553, Medical, 1857–, letter from William McCrea, president CBH, to chief secretary, 2 October 1857.
[51] PROV, VPRS 1189/P0 Chief Secretary’s Department, Inward Correspondence 1, Unit 554, Medical, 1858–, letter from William McCrea, president CBH, to chief secretary, 15 April 1858.
[52] PROV, VPRS 1189/P0 Chief Secretary’s Department, Inward Correspondence 1, Unit 554, Medical, 1858–, letter from William McCrea, president CBH, to chief secretary, 18 February 1858.
[53] PROV, VPRS 1189/P0 Chief Secretary’s Department, Inward Correspondence 1, Unit 554, Medical, 1858–, letter from William McCrea, president CBH, to chief secretary, 10 February 1858.
[54] PROV, VPRS 1189/P0 Chief Secretary’s Department, Inward Correspondence 1, Unit 554, Medical, 1858–, CBH expenses, April 1858.
[55] Letter from Fred Thomas, 5 October 1857.
[56] Victoria, Central Board of Health report of the board for the year 1872, Government Printer, Melbourne, 1873, p. 6.
[57] ‘The reported case of small-pox at Ballaarat’, Argus, 30 April 1858, p. 5; ‘The small-pox on Ballarat’, Star, 28 April 1858, p. 2; ‘The reported small-pox’, Star, 29 April 1858, p. 2; ‘Eastern Municipal Council’, Star, 29 April 1858, pp. 2-3; Keith Macrae Bowden, Goldrush doctors at Ballaarat, Magenta Press, Mulgrave, 1977, p. 72.
[58] Dorothy Green, ‘Anti-vaccination and syphilis’, Medical Journal of Australia, 7 March 1970, p. 500.
[59] PROV, VPRS 1189/P0 Chief Secretary’s Department, Inward Correspondence 1, Unit 554, Medical, 1858–, letter from William McCrea, president CBH, to chief secretary, 28 April 1858.
[60] Victoria, Central Board of Health third annual report, p. 4.
[61] PROV, VPRS 1189/P0 Chief Secretary’s Department, Inward Correspondence 1, Unit 553, Medical, 1857–, letter from William McCrea, president CBH, to chief secretary, 11 November 1857.
[62] PROV, VPRS 1189/P0 Chief Secretary’s Department, Inward Correspondence 1, Unit 553, Medical, 1857–, letter from William McCrea, chief medical officer, to chief secretary, 1 October 1857.
[63] ‘Municipal Council East’, Star, 15 July 1857, p. 3.
[64] ‘The committee of the Benevolent Asylum and Dr Bunce’, Star, 25 November 1862, p. 1S.
[65] Evans, ‘Vaccine lymph’, p. 167.
[66] ‘Variola or varicella’, Australian Medical Journal, January 1869, p. 27.
[67] McWhirter, ‘Lymph or liberty’, p. 49.
[68] ‘Social’, Star, 23 July 1863, p. 1S.
[69] Victoria, Central Board of Health, Fourth annual report under the Act 18 Victoria, No. 13, Government Printer, Melbourne, 1859-1860, p. 4.
Material in the Public Record Office Victoria archival collection contains words and descriptions that reflect attitudes and government policies at different times which may be insensitive and upsetting
Aboriginal and Torres Strait Islander Peoples should be aware the collection and website may contain images, voices and names of deceased persons.
PROV provides advice to researchers wishing to access, publish or re-use records about Aboriginal Peoples